At a time when healthcare is at a crossroads, the "Global State of Patient Safety 2023 – Supporting Leaders" seminar hosted by SHARE - Centre for Resilience in Healthcare, served as the perfect precursor to the week-long kick-off of the EU project, Support4Resilience.
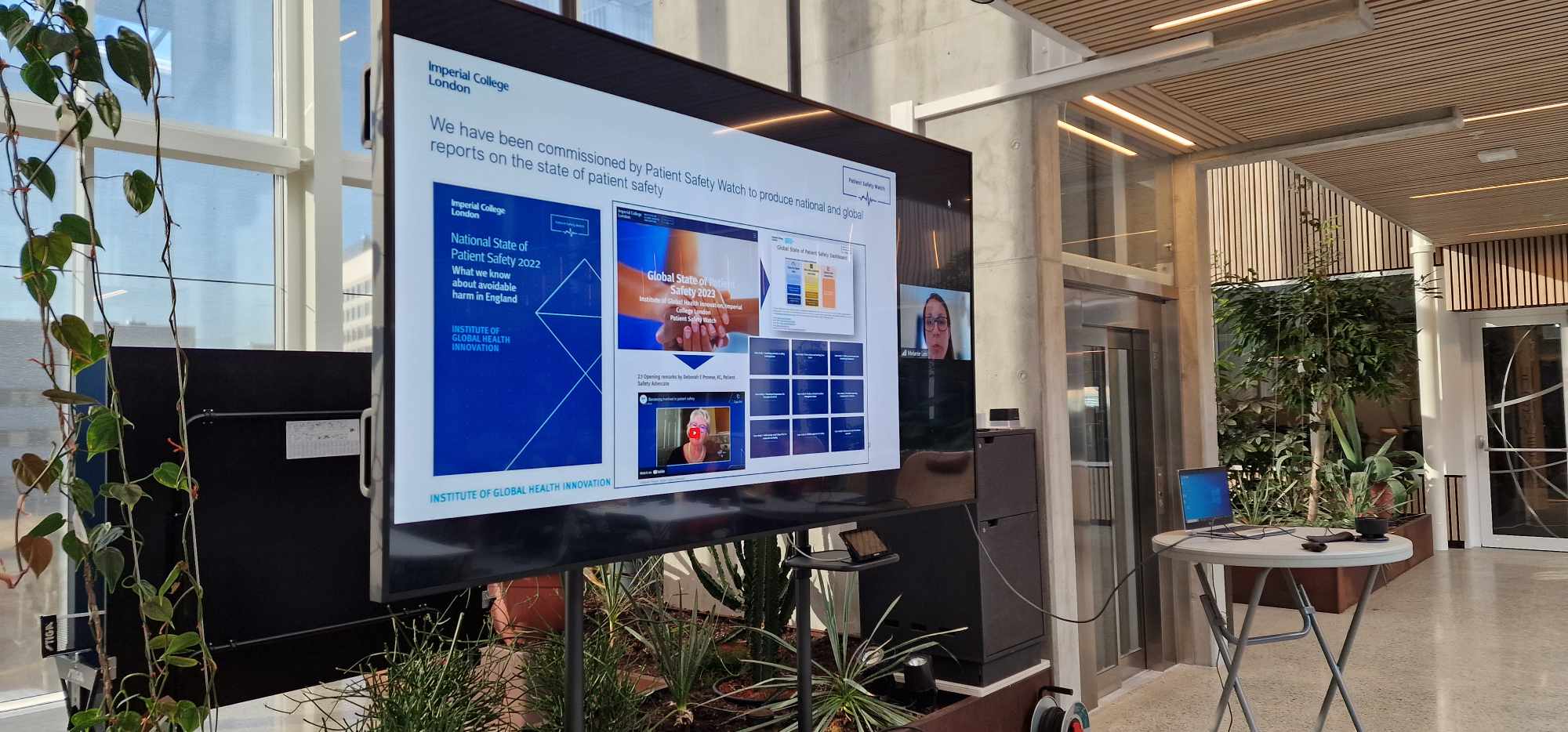
The report, Global State of Patient Safety 2023, from the Institute of Global Health Innovation at Imperial College, London shows that Norway ranks number one in the world. We gathered some of the world's leading thinkers and practitioners in patient safety for a more nuanced examination of this achievement, and how this position could be maintained by continued focus on leadership, workforce dynamics, and the invaluable contributions of informal caregivers.
The seminar began with an introduction by Prof. Siri Wiig, the principal investigator of the EU Horizon Europe funded program, Support4Resilience, set to launch next week. Prof. Wiig outlined the project's objectives, focusing on the development of a digital toolbox tailored for leaders in elderly care. The project aims to strengthen the resilience and mental well-being of both healthcare staff and informal carers by addressing key challenges in the healthcare sector, such as labor shortages and high levels of stress. By improving work conditions, providing training, and promoting efficient use of resources, the toolbox seeks to offer evidence-based approaches to ensure high-quality care. Scheduled for testing in six European countries and Australia, the project aims to improve healthcare quality, enhance employee satisfaction, and boost motivation.
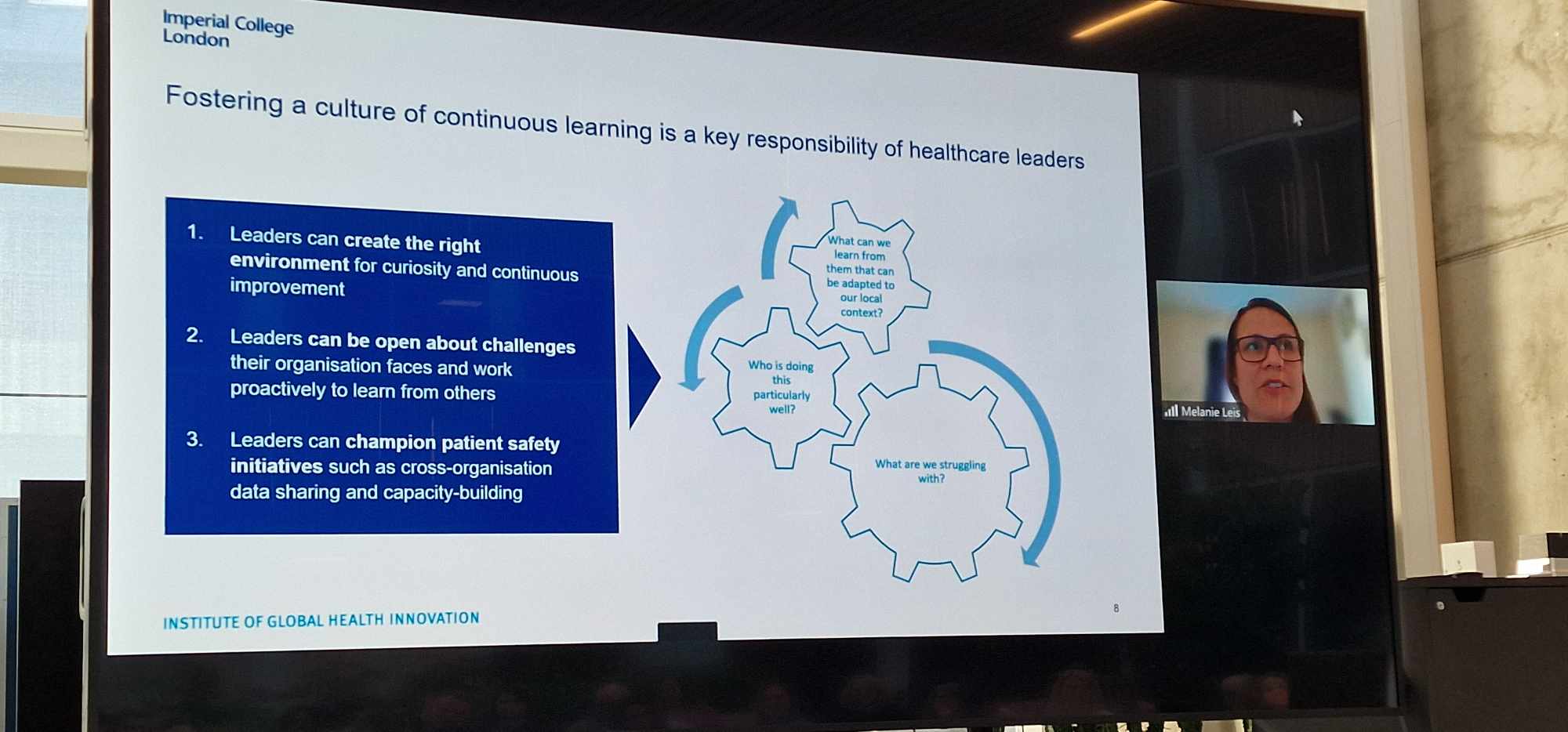
Wiig linked the project's goals to insights from the Global State report, highlighting how empowering leaders to lead patient safety initiatives can lead to widespread performance improvements. By emphasizing learning, ongoing enhancement, and fostering a safety-oriented culture, this strategy has the potential to increase worker satisfaction and retention, consequently raising the standard of patient care and safety.
Melanie Leis, project lead for the report on Global State of Patient Safety 2023, og senior adviser Dr. Mike Durkin, both from Global Health Innovation at Imperial College joined the seminar online. Leis explained how the report employs four critical patient safety indicators: Maternal Mortality, Treatable Mortality, Adverse Effects of Medical Treatment, and Neonatal Disorders. These indicators offer a thorough and reliable perspective on patient safety, concentrating on preventive measures and responses to healthcare challenges. However, she was quick to point out how variations in these indicators could obviously impact Norway's standing in patient safety rankings.
Both Leis and Durkin highlighted the importance of including patient and family insights for better patient safety, pushing for more transparent and broader data collection for analysis and learning. Stressing on the need for real-time, accurate data and patient perspectives, they emphasized continuous learning, openness, and collaboration across healthcare organizations, underlining trust, empathy, and problem-solving as key leadership qualities, along with top management's dedication to patient care. The role of AI in safety improvements, the need for adapted safety measures in home-based care, and the importance of reliable government data for transparency and care effectiveness are also discussed.
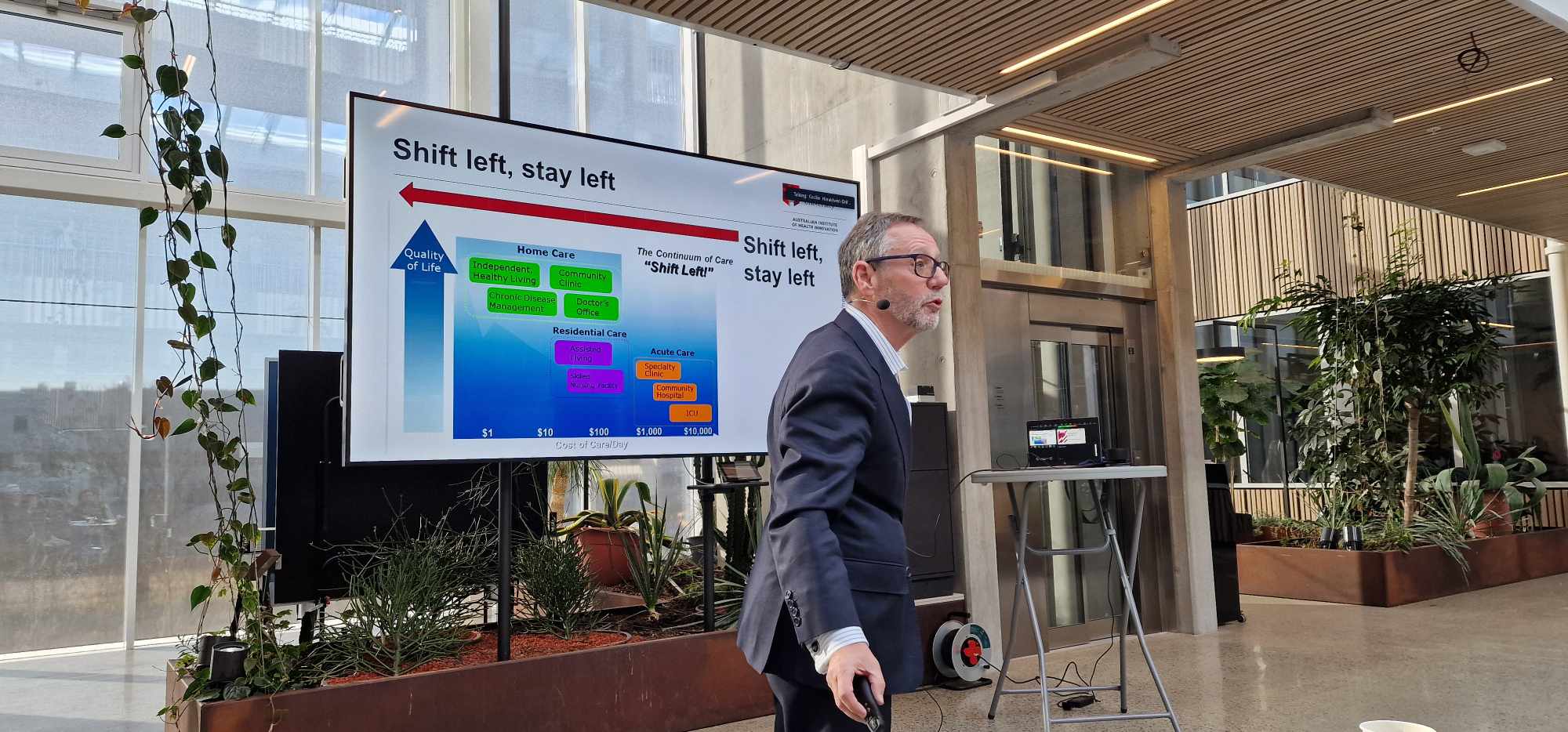
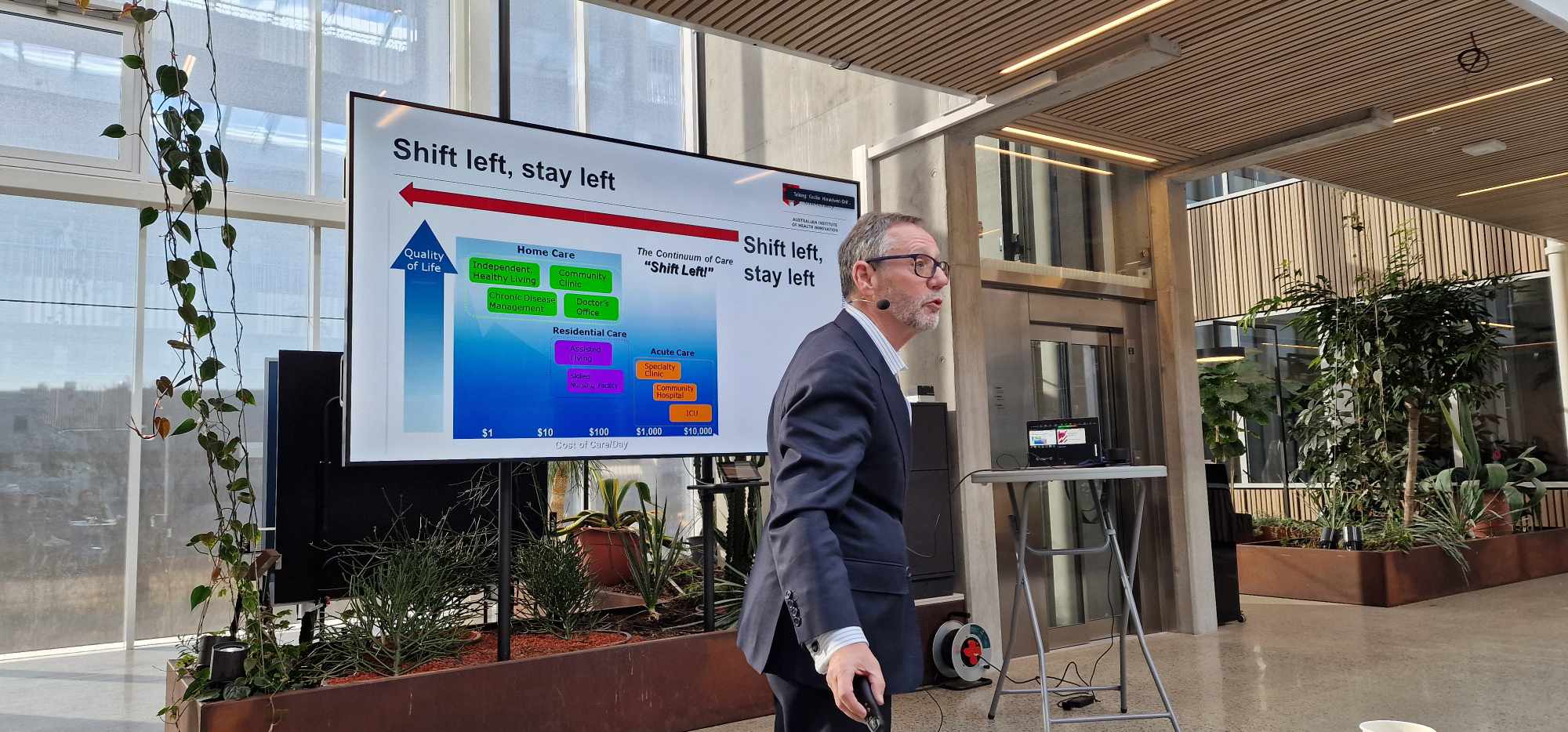
Their points were supported by the final speaker, Prof. Jeffrey Braithwaite from the Australian Institute of health Innovation, who focused on the necessity of considering various perspectives in ranking healthcare systems by patient safety and efficiency, highlighting the importance of accurate patient safety indicators and data reporting by countries. He discusses the challenge of sustaining high healthcare rankings, using Norway as a case study for ongoing improvement efforts. Braithwaite acknowledged that healthcare often moves forward despite policy, illustrating the difference between "Work as Done" and "Work as Imagined." He suggests enhancements for health systems through initiatives like the 60:30:10 framework to balance care delivery and minimize procedural waste. He concluded by identifying responsive management, effective leadership, and strong interdisciplinary teamwork as traits of high-performing health systems.
It is clear that the path to improved patient safety and healthcare efficiency requires a concerted effort. It demands leadership that is empathetic, transparent, and committed to continuous learning and improvement. It calls for systems that not only adapt to the challenges of today but are also resilient enough to meet the demands of tomorrow.
.