SHARE - Centre for Resilience in Healthcare recently gathered researchers and health care professionals to an open seminar about the future of leadership in healthcare. The seminar concludes a full week of activities related to the Support4Resilience project.
European elderly care experiences labor shortages, lack of qualified healthcare workers and a major mismatch of capacity and demands in healthcare services, causing stress, burnout, and reduced mental health and wellbeing among healthcare workers, leaders, and informal caregivers across the world.
In this seminar a wide selection of international guest speakers talked about topics related to how we can meet and overcome these challenges.
"We are so delighted to bring these international highly esteemed researchers, policy makers and patient advocates to Stavanger as part of the Support4Resilience kickoff. It is a privilege to host an open seminar where their voices give us different perspectives on the future of leadership in healthcare", says Siri Wiig, centre director of SHARE - Centre for Resilience in Healthcare at the University of Stavanger.
This topic is important in an international setting and in a local setting.
"We need to discuss these challenges and potential solutions. I would like to thank the speakers and the participants for coming, and my colleagues for the tremendous organizing", she adds.
Managing risk in hazardous conditions
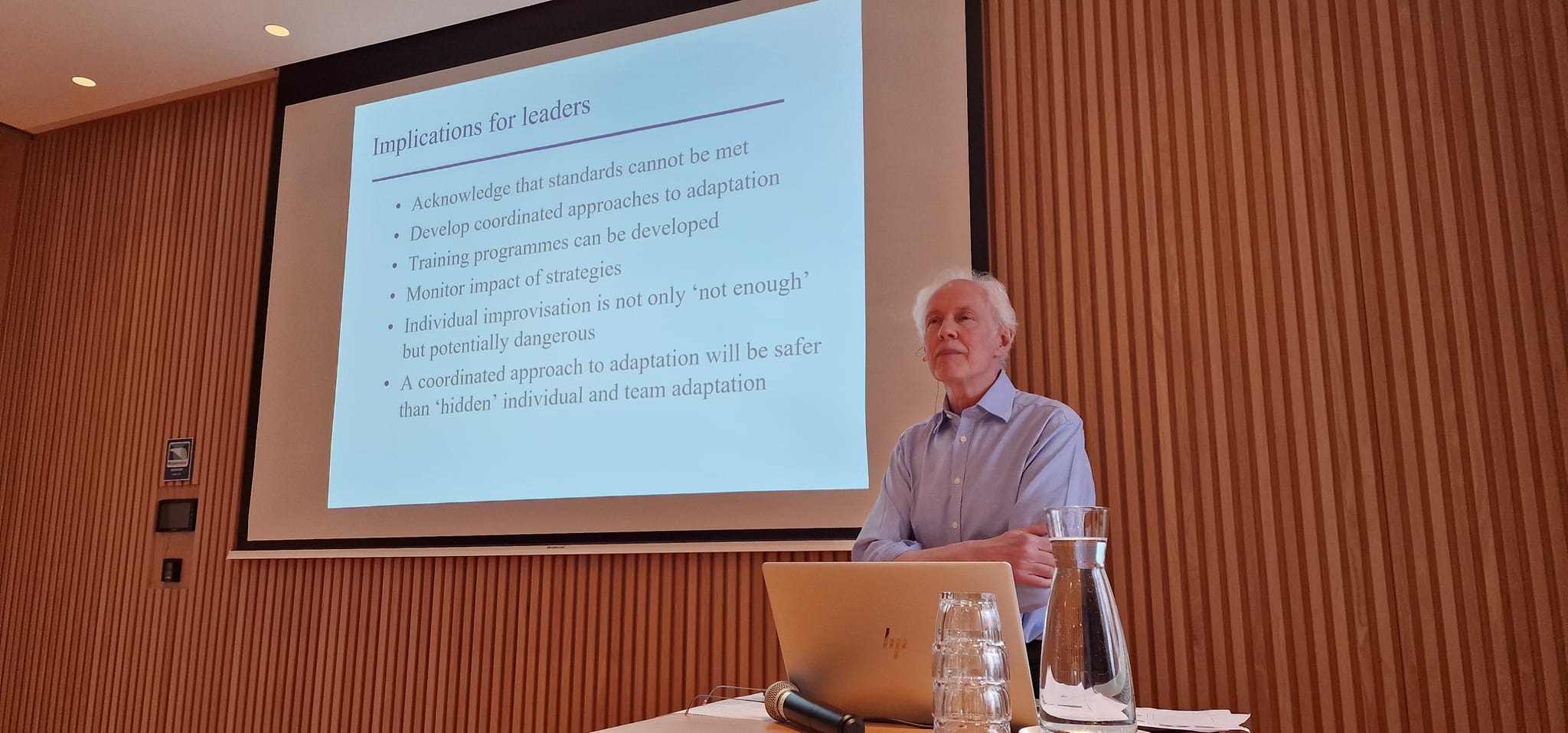
In his presentation, Charles Vincent, Professor at the University of Oxford, England, discussed the challenges of addressing human error in healthcare and the need for strategies to adapt and improve safety and quality. He emphasized the importance of studying resilience and strategies for managing errors. Vincent presented a paper titled "Improvisation is not enough," focusing on adapting in healthcare, particularly in intensive care settings. Vincent emphasized the need for both short-term and long-term strategies to manage errors effectively.
He highlighted the gap between desired standards of care and the reality faced by healthcare providers, stressing the importance of managing this gap effectively. He proposed a framework for understanding adaptation strategies, including anticipatory measures and on-the-day adjustments. Vincent stressed the importance of leadership in promoting openness and ongoing training and monitoring to enhance resilience and ensure better patient outcomes. He urged leaders not to abandon long-term strategies despite the immediate pressures of day-to-day operations.
Sustaining change through leadership
Catherine Calderwood, Professor at the University of Strathclyde and former Chief Medical Officer for Scotland, reflected on her experience with the Morecambe Bay Investigation on the maternity and neonatal services in Morecambe Bay NHS Foundation. She emphasizes the importance of listening to both patients and staff within healthcare organizations. She described a case where standards were not being met and adaptations led to unsafe practices, highlighting issues with communication and tolerance of exceptions.
Despite a seemingly normal perinatal fatality rate, the nature of the deaths raised concerns. Calderwood stressed the need for care and compassion in patient interactions, citing instances where families felt neglected or deceived. She calls for a culture of support and openness within workplaces and suggests that leadership plays a crucial role in fostering such environments. Finally, she acknowledged the challenges faced by healthcare professionals, particularly due to increasing pressures and demands.
Measuring resilience and mental well-being
Louise Ellis is a senior researcher representing the Australian Institute of Health Innovation at Macquarie University. She shared insights about her research related to measuring support for resilience and mental wellbeing. She discussed the concept of resilience in healthcare systems, emphasizing the importance of distinguishing between individual and systems resilience. She highlighted the challenges and initiatives in measuring and improving resilience, particularly in the context of the COVID-19 pandemic.
The focus of her research is on developing tools to assess and enhance resilience at various levels, from individual well-being to organizational culture, with the aim of reducing staff burnout, improving psychological safety, and enhancing patient care. She outlined a methodology involving data collection, validation, and intervention implementation, with a broader goal of transforming workplace culture and prioritizing team collaboration. She concluded her presentation with a discussion on future steps, including validation across different countries and sectors, and the evaluation of intervention effectiveness.
Widening the horizon of healthcare
Martin Hatlie, Founding Member of Patients For Patient Safety USA, talked about the importance of leadership to support patients’ and families’ resilience and mental wellbeing. He talked about his global advocacy work with the World Health Organization (WHO) and Patients For Patient Safety, which is a network of people and organizations focused on making healthcare safe in the United States. The network is led by people who have experienced medical error as a patient or in their families.
The seminar concluded with a panel discussion among the speakers.